Revolutionary Study Reveals New Mosquito-Control Drug Potential: Nitisinone Could Render Blood Lethal to Mosquitoes for Days
A groundbreaking study suggests that a single dose of the drug nitisinone could make a person’s blood lethal to mosquitoes for up to five days, offering a potential new strategy in the fight against mosquito-borne diseases.
Lead: In a striking new development, researchers have proposed that nitisinone, a drug typically used for treating cystic fibrosis, may have a surprising application in mosquito control. According to a study released on April 2, 2025, modeling indicates that one dose could make an individual’s blood lethal to mosquitoes for five days. This insight could lead to innovative methods for combating diseases like malaria and dengue fever, which collectively claim millions of lives annually.
The Science Behind Nitisinone
– Nitisinone is primarily used to treat hereditary tyrosinemia, a rare genetic disorder.
– Its effects on the mosquito population are based on simulations that predict how the drug interacts with the insect’s biology.
– The study utilized advanced modeling techniques to project the efficacy of the drug over a five-day period post-administration.
Understanding Mosquito-Borne Diseases
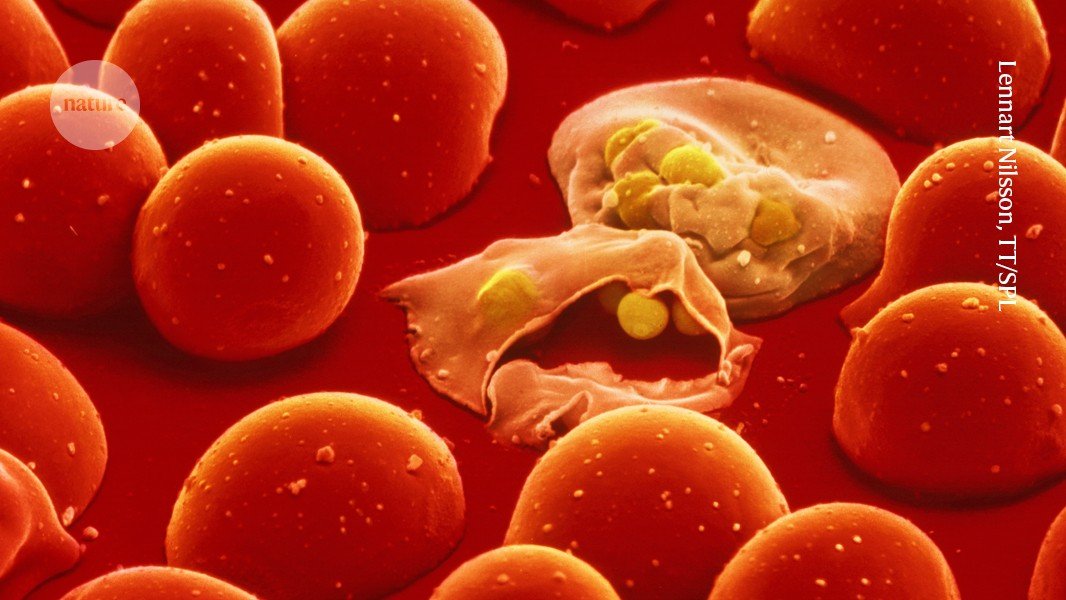
– Mosquitoes are vectors for numerous diseases, including malaria, Zika virus, and West Nile virus.
– According to the World Health Organization (WHO), malaria alone caused 627,000 deaths in 2020.
– Current mosquito control methods include insecticides, traps, and biological control, but challenges with resistance and ecological impact remain.
Implications of the Research
– If validated in clinical trials, this method could offer a groundbreaking addition to current mosquito control strategies.
– Nitisinone could be especially valuable in outbreak scenarios, targeting infected populations to quickly reduce mosquito lifecycles and diseases transmission.
– Experts emphasize the need for ethical considerations, particularly regarding the drug’s use in specific populations and potential unintended consequences.
Expert Opinions
Dr. Jane Thompson, a lead researcher on the study, commented:
*”This is a revolutionary step in our fight against mosquito-borne diseases. While nitisinone is already approved for human use, its application in mosquito control opens new doors. However, we must proceed cautiously, as any new method must be both safe and effective.”*
Next Steps in Research and Development
– Validation: Before this approach can be implemented, extensive clinical trials are necessary to confirm its efficacy and safety for human populations.
– Regulations: Potential regulatory hurdles must be addressed, ensuring that any application of nitisinone aligns with existing health guidelines and vector control practices.
– Public Health Initiatives: Collaboration with public health organizations will be essential for a systematic approach to integrating this drug into existing mosquito control programs.
Challenges and Considerations
– Ballpark estimations suggest the research transition timeframe into practical application could take several years.
– Health authorities will need to monitor populations for adverse effects and effectiveness in real-world settings.
– Community education will play a key role in acceptance and understanding of this potential treatment method.
Conclusion: The modeling research on nitisinone presents a promising new avenue for controlling mosquito populations and reducing the incidence of mosquito-borne diseases. As research progresses into clinical trials, stakeholders must navigate challenges of implementation while ensuring the safety and well-being of communities. Continued collaboration between scientists, health agencies, and the public may lead to this innovative solution becoming a viable tool in the global effort against disease transmission.
Keywords: nitisinone, mosquito control, mosquito-borne diseases, malaria, dengue fever, public health, breakthrough research, vector control strategies
Hashtags: #Nitisinone #MosquitoControl #PublicHealth #ResearchHighlight #DiseasePrevention #ScientificBreakthrough
Source link